Optical Coherence Tomography Guided Robotic Ophthalmic Surgery
Active Personnel:
- Haoran Yu 2010-present
Project Description:
Retinal procedures require high precision, stability and intra-ocular dexterity. As new surgical approaches are introduced, new demand for enabling technology also grows. Ophthalmic surgeons, especially retina specialists, are among the surgeons that must meet strict demands for hand stability and precision. However, increased physiological tremor and a decrease in vision are inevitable for most humans throughout time. Hence, involving surgical robots with emerging technology on visual feedback seems to be a potential way to augment surgeons' expertise with steadiness and precision of robots. Robots are required to ensure safe ocular and intra-ocular manipulation with tremor cancellation, stable output, high precision and high repeatability. And imaging technologies should provide micron level visual feedback to help guide both the surgeon and the robot.
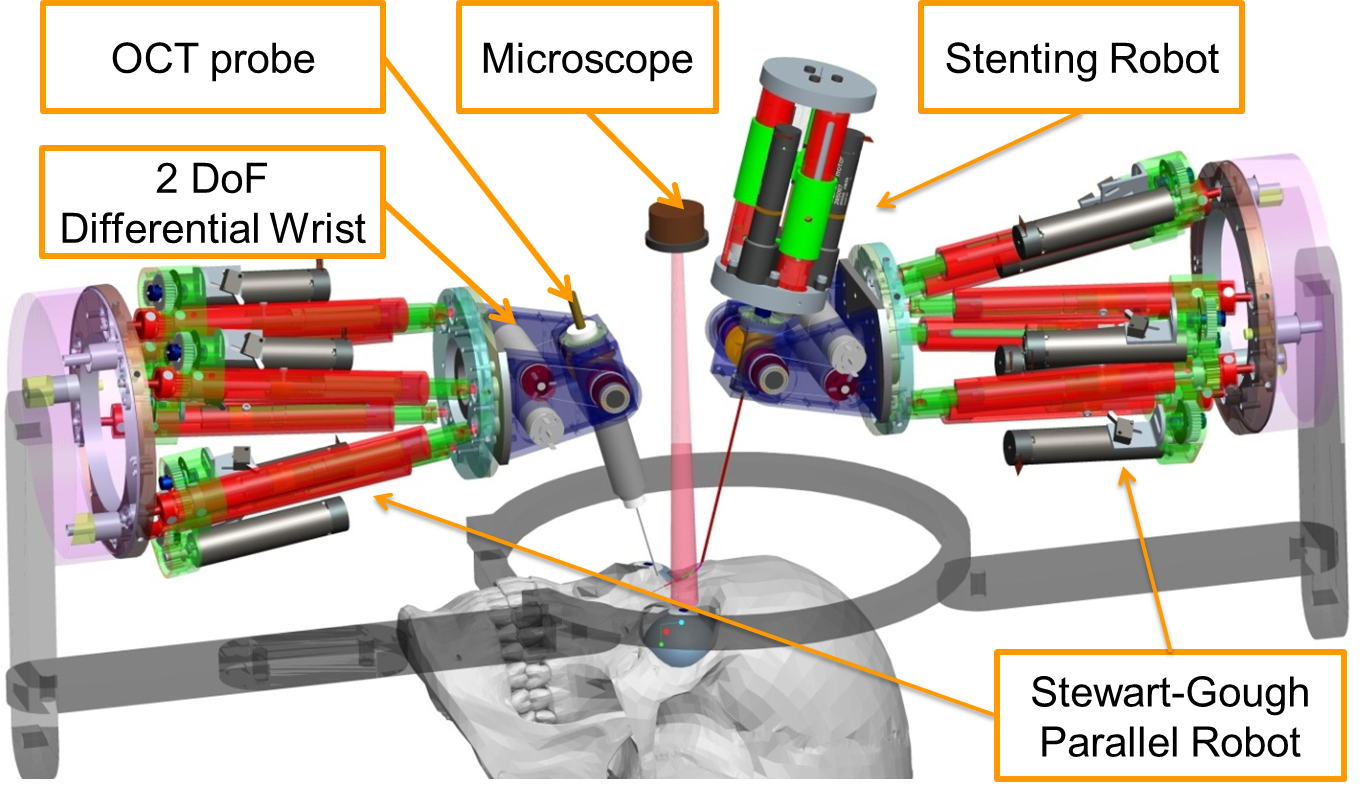
We developed a surgical prototype for dual-arm robotic surgery with Optical Coherence Tomography (OCT) guidance. The key research goals address integration, calibration and control of the 22-DOF dual arm robotic surgical system, calibration of a customized B-mode OCT probe, OCT to robot hand-eye registration, feasibility study of the influence of the OCT probe and the robot on surgical interventions, and assistive telemanipulation and 3D OCT-microscope visual based virtual fixtures for retinal procedures including cannulation, stent deployment and ILM membrane peeling.
System Setup and OCT Probe:
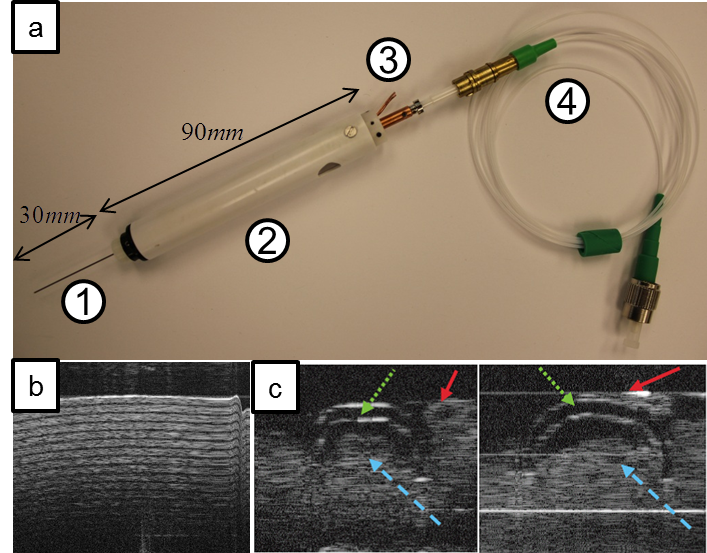
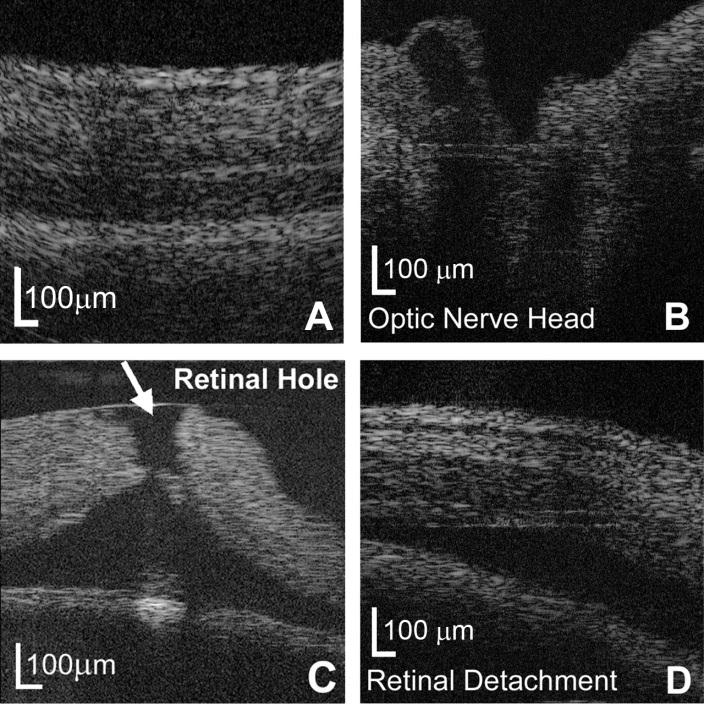
The surgical system contains up to 22 DoF with 6 DoF Stewart-Gough Parallel Robot, 2 DoF Differential Wrist and 3 DoF Intra-ocular Dexterous Robot. The miniature B-mode OCT probe has a 0.51mm scanning tip in diameter with a scanning fequency upto 30 Hz. The axial resolution of the real-time OCT image is 4-6 microns and the lateral resolution is 25-35 microns and 32-45 microns at the scanning edge. The B-mode OCT image has 1-2 mm penetration depth into the retina and the scanning beam is focused at the working distance 3-4 mm away from the probe.
|
|
|
|
Robot Setup for an Ophthalmic Surgery |
(a) B-mode OCT Probe and OCT images: (b) Cellophane tape (c-d) Bridge separator |
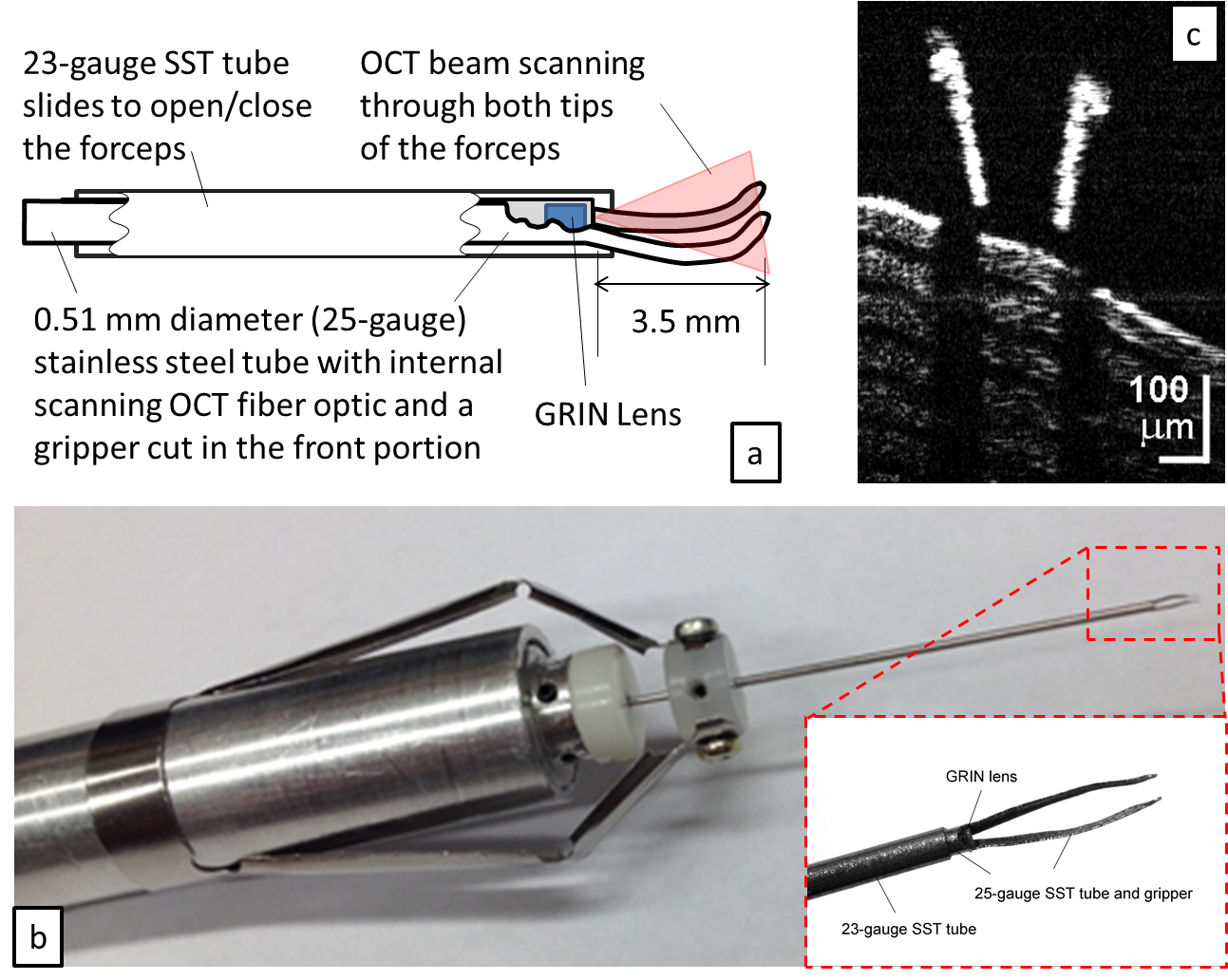
A miniature B-scan OCT probe uniquely combined with an ophthalmic surgical forceps was designed with the probe positioned within the forceps rather than a forceps positioned within or adjacent to the OCT probe. The forceps tips were fabricated to be aligned with the cross-sectional center of the probe, and located 3.5 mm distal to the OCT tip to be at the best focal point position. A 23-gauge extra-thin wall SST was used to slide up and down the outside of the 25-gauge tube to cause opening and closure of the gripper manually. The OCT forceps may be used as either a hand-held instrument or integrated within a robotic system.
 |
|
| B-mode OCT pictures of Retina | OCT-forceps probe design with OCT images of the probe's tips. |
Robotic+OCT Guidance Evaluation:
Ophthalmic retinal surgery is carried out under a microscope visualization. One of the challenges facing surgeons is the ability to gauge depth via narrow baseline stereo visualization. The challenge often requires surgeons to use visual cues such as the tool shadow to discern distance from the retina. In addition, certain anatomy such as the internal limiting membrane or the epiretinal membrane are thin and transparent to the naked eyes. Surgeons have resorted to visualization aids through the use of triamcinolone powder to help visualize the first instant when the gripper disturbs the membrane. We carried out a series of experiments to address one fundamental question: what is the relative importance of robotic assistance with and without depth feedback using OCT visualization? To answer this question we design a study that tests different combinations of robotic assistance and OCT feedback and compare surgeon performance with and without robot or OCT visualization aids.
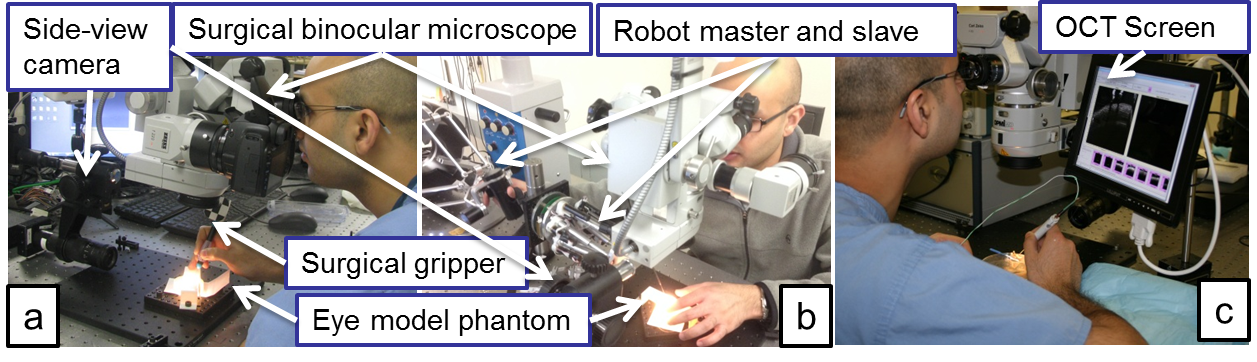 |
| An ophthalmic fellow performing ophthalmic interventions on different setup |
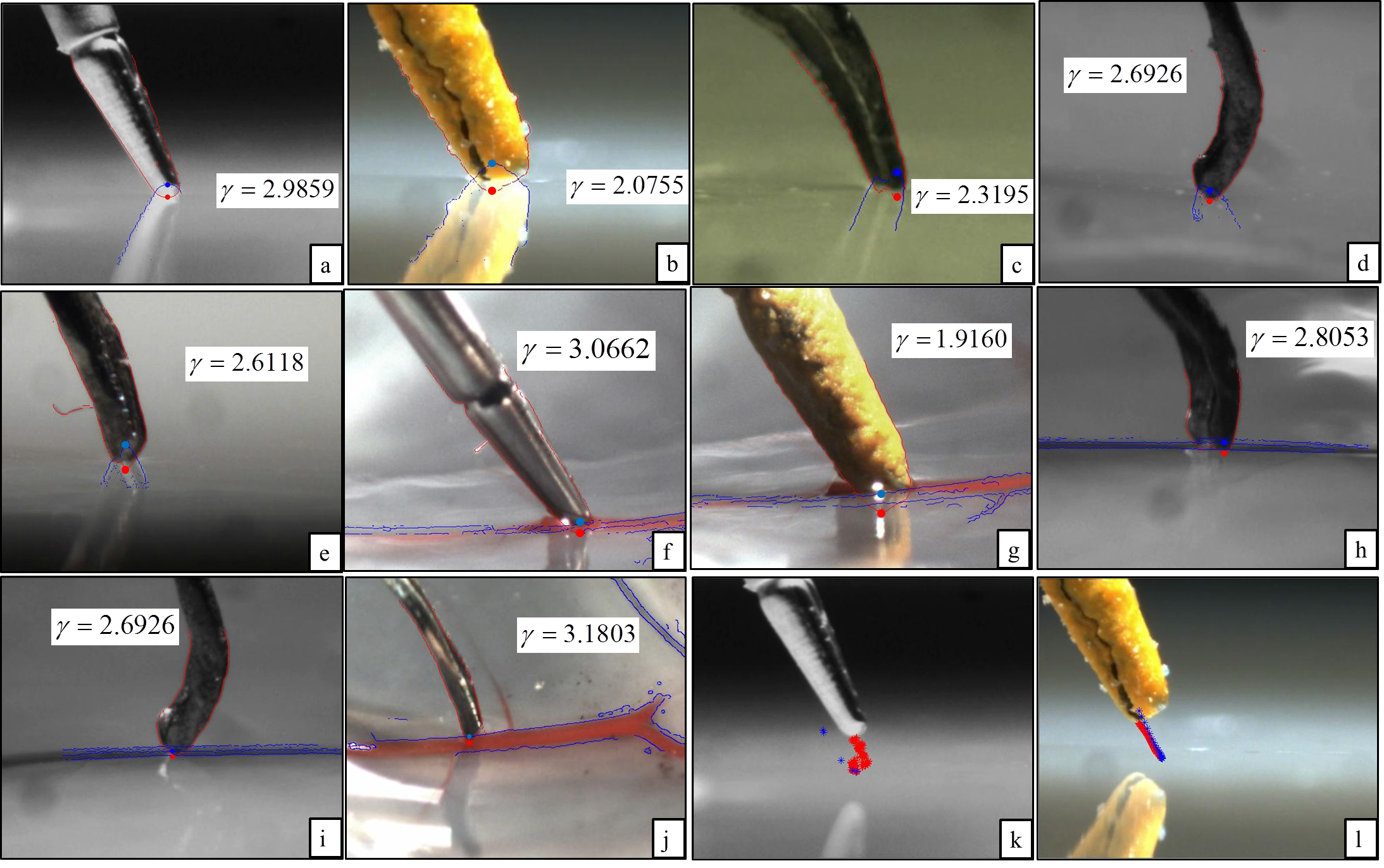 |
| Side View of Approaching task on different experimental conditions |
 |
| Side view of membrane peeling task on different experimental conditions |
The experimental evaluations of approaching and membrane peeling were carried out on both phantom model and real eye with and without OCT guidance or robotic assistance. The results show that only when robotic assistance and OCT guidance are combined together, the surgical performance would be significantly better than other experimental conditions.
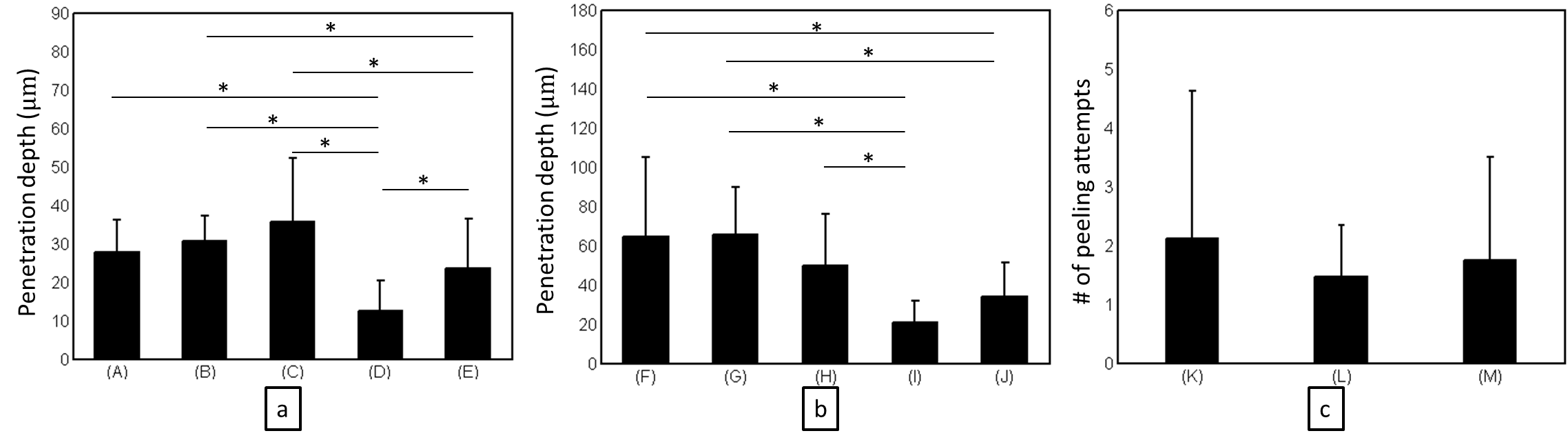 |
| Anova on different experimental setup with different experimental conditions |
Publications
- Yu, H., Shen, J. H., Joos, K. M., and Simaan, N. (2015), "Calibration and Integration of B-mode Optical Coherence Tomography for Assistive Control in Robotic Micro-surgery", In preparation to submit to ASME/IEEE Transaction on Mechatronics, 2015.
- Yu, H., Shen, J. H., Shah, R. J., Simaan, N., and Joos, K. M. (2015), "Evaluation of microsurgical tasks with OCT-guided and/or robot-assisted ophthalmic forceps", Biomedical Optics Express, Vol. 6, No. 2, pp. 457--472, 2015.
- Yu, H., Shah, R. J., Shen, J. H., Joos, K. M. and Simaan, N. (2014). "Preliminary Evaluation of a Robotic Retinal Surgical Manipulator", In 2014 The Association for Research in Vision and Ophthalmology Annual Conference (ARVO'2014).
- Yu, H., Shen, J. H., Joos, K. M. and Simaan, N. (2013). "Design , Calibration and Preliminary Testing of A Robotic Telemanipulator for OCT guided Retinal Surgery". IEEE International Conference on Robotics and Automation (ICRA), pp.225-231, 2013.
- Shen, J. H., Yu, H., Simaan, N. and Joos, K. M. (2013). "A Robotic-controlled Intraocular OCT Probe", Investigative Ophtalmology and Visual Science, Vol 54, No. 6, pp. 1502, 2013.
- Joos, K. M., Shen, J. H. (2013). "Miniature real-time intraoperative forward-imaging optical coherence tomography probe", Biomedical Optics Express, 4(8):1342-50, January 2013.
- Shen, J. H., Kozub, J., Prasad, R., and Joos, K. M. (2011). "An Intraocular OCT Probe". Invest. Ophthalmol. Vis. Sci., 52: E-Abst, 2011.
Collaborators:
Dr. Karen M. Joos & Dr. Jin-Hui Shen
Vanderbilt Eye Institute, Vanderbilt University.
Acknowledegment:
This project was funded by the Vanderbilt Discovery Grant 4229990095. The project name is ''OCT-Assisted Robotic Micro-Vascular Retinal Surgery''.
Haoran Yu was also funded by Vanderbilt Institute in Surgery and Engineering (ViSE) fellowship during 2014/2015 academic year.